Learning objectives:
On completion of this case study, the student/reader will be able to:
- Describe the etiology of Streptococcus pneumonia infection.
- Explain the clinical manifestations of Streptococcus pneumonia infections.
- Identify available treatment options and interventions to prevent Streptococcus pneumonia.
History:
A 54-year-old white male was seen in the emergency department. He gave a history of homelessness and chronic alcoholism. His symptoms included fever, chills, and a deep productive cough. The patient was hospitalized for 3 days. The patient possibly has a bacterial infection due to the high white blood count along with neutrophilia, and lymphocytopenia and the observed toxic changes in the white blood cells. The patient also has low red blood cell count and observed macrocytosis morphology, indicating possible anemia caused by chronic alcoholism.
Save your time!
We can take care of your essay
- Proper editing and formatting
- Free revision, title page, and bibliography
- Flexible prices and money-back guarantee
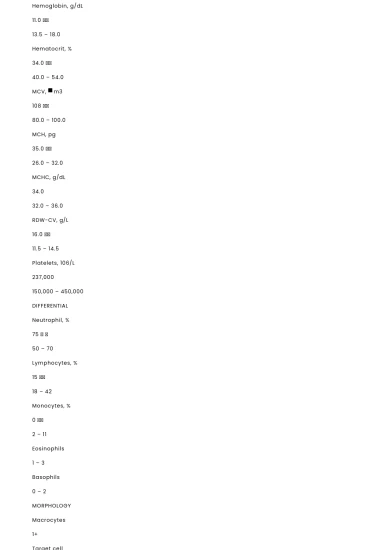
Table 1 – Blood Analysis Results
CBC RESULTS
VALUE
REFERENCE RANGE1
WBC, μL
18,300 ↑↑
3,600 -10,600
RBC, x106/μL
3.9 ↓↓
4.7 – 6.1
Hemoglobin, g/dL
11.0 ↓↓
13.5 – 18.0
Hematocrit, %
34.0 ↓↓
40.0 – 54.0
MCV, μm3
108 ↑↑
80.0 – 100.0
MCH, pg
35.0 ↑↑
26.0 – 32.0
MCHC, g/dL
34.0
32.0 – 36.0
RDW-CV, g/L
16.0 ↑↑
11.5 – 14.5
Platelets, 106/L
237,000
150,000 – 450,000
DIFFERENTIAL
Neutrophil, %
75 ↑ ↑
50 – 70
Lymphocytes, %
15 ↓↓
18 – 42
Monocytes, %
0 ↓↓
2 – 11
Eosinophils
1 – 3
Basophils
0 – 2
MORPHOLOGY
Macrocytes
1+
Target cell
Occasional
Toxic granulation
Observed
Vacuolization
Observed
Döhle bodies
Observed
Abbreviations: WBC, white blood cell; RBC, red blood cell; MCV, mean corpuscular volume; MCH, mean hemoglobin value; MCHC, mean corpuscular hemoglobin volume, RDW-CV, red blood cell distribution width.
Table 2 – Bacterial Culture Results
Gram Stain
Gram-positive lancet-shaped diplococci
Culture/Colony Morphology
Alpha-hemolytic round, glistening, dome-shaped appearance
Biochemical Test
Bile Solubility – positive
Optochin susceptibility sensitive 5.0
Discussion
Clinical Manifestations and Etiology
Streptococcus pneumoniae is one of the major pathogens infecting humans worldwide. S. pneumoniae most commonly affects children, the elderly, and other people with weakened immune systems. It is the most common cause of community-acquired bacterial pneumonia.2 Streptococcus pneumonia can cause many types of illness including pneumonia, ear infections, sinus infections but can also lead to severe cases of meningitis and sepsis.2,3
Pneumococcal infection is spread from respiratory droplets from the nose or mouth of an infected person. Droplets in the air may be inhaled by those nearby. Contact with hands, tissues, and other articles contaminated by infected nasal and oropharyngeal secretions also spreads the infection.3,4
S. pneumoniae is normally found in the nasopharynx approximately 5-10% of healthy adults and approximately 20- 40% of healthy children.4 Crowded environments (e.g. daycare centers, army barracks, etc.) increase the potential for exposure to S. pneumonia. The pneumococcus attaches to the nasopharyngeal cells through interaction of bacterial surface adhesins. This normal colonization can become infectious if the organism is carried into areas such as the canal that connect the middle ear to the nasopharynx or nasal sinuses, where it can cause otitis media and sinusitis.2,4
[bookmark: _Hlk3490018]S. pneumonia produces a variety of virulence factors, including the polysaccharide capsule, surface-associated proteins and enzymes, and the toxin pneumolysin (PLY). The most important virulence factor of the pneumococcus is the polysaccharide capsule. The capsule enhances the ability of bacteria to prevent phagocytosis by preventing complement C3b opsonization of the bacterial cells.5,6 The capsule and surface protein that interfere with phagocytosis help the microorganism attack the host immune’s defense. The infection causes inflammation, one of the main symptoms of S. pneumonia. Autolysis causes lysing of bacteria producing inflammation which involves complements of the cell wall and the toxin pneumolysin.5,6
Streptococcus pneumonia symptoms include shaking, fever, low blood pressure, shortness of breath, and rapid breathing, symptoms similar to those observed in the patient.2 (Refer to patient history). The patient’s CBC (Table 1), indicated elevated white count, decreased lymphocytes, and increased neutrophils with toxic changes. These are all indicators of a bacterial infection such as S. pneumonia. Neutrophil’s primary function is phagocytosis of organisms and other infectious agents. A “left shift” to more immature neutrophil forms occurs as precursors are released from the bone marrow during infection.1,7
Toxic granules, Döhle bodies, and vacuoles noted in the patient’s peripheral blood smear most likely result from the activation of increased cytokine activity and shortened activity of neutrophils during infection (Table 1). In many infections or toxic stimulations, neutrophils respond with large dark blue intracytoplasmic azurophil granules.1,7 The toxic granules may be present within metamyelocytes, band, and segmented neutrophils in such cases. Toxic granulation would appear in the neutrophil's cytoplasm which reflects an increase in lysosomal enzyme and primary azurophilic granules. Toxic granulation is seen in cases of severe infection, as a result of phagocytosis. Infection is the most frequent cause of toxic granulation. 1,7 Toxic granulation may be observed in the band neutrophil shown in Image 1.9 Döhle bodies are small, light blue-gray irregular staining patches of cytoplasm seen near the edge of the cell in granulocytes in certain conditions. Associated with infections, burns, leukemia, chemotherapy, inflammatory state. Döhle bodies are present when the body is responding to unusually severe stress or stimulus. This stress may cause the cytoplasm of some cells to mature improperly. When present, they are typically observed in the outer periphery of the cytoplasm, close to the cell wall. Döhle bodies are composed of RNA from rough endoplasmic reticulum, which is left over from previous maturation stages. Their presence does not aid in the diagnosis of the disorders in which they are found, but they are frequently seen along with toxic granulation and/or vacuoles in cases of infections or burns. (7,8) Döhle bodies are indicated by the arrows in Image 2.7 Vacuoles are clear, unstained areas in the cytoplasm of neutrophils and seen in conditions such as infection when toxic granulation and Döhle bodies are present. Toxic vacuolization is indicated by the arrows in the cell of Image 3.7 Toxic vacuolation and toxic granulation are classified as reactive and not pathologic since the body is responding normally in an effort to rid itself of the infection caused by bacteria.1,7
The observed decrease in red blood cells, hemoglobin, hematocrit, and increase in MCV, MCH, and RDW can be associated with the patient’s history of alcoholism (Table 1). Chronic excessive alcohol ingestion reduces the number of blood cell precursors in the bone marrow and causes characteristic structural abnormalities in these cells, resulting in fewer-than-normal or nonfunctional mature blood cells.8 For example, enlarged RBCs can occur in the blood - a condition called macrocytosis — as well as oddly shaped RBCs that are subject to premature or accelerated destruction because of their structural abnormalities. As a result, alcoholics frequently are diagnosed with anemia.8 Macrocytosis is used to describe erythrocytes that are larger than normal, typically reported as mean cell volume (MCV) greater than 100fL. The amount of hemoglobin increases proportionately with the increase in cell size. Increased MCV is an indication of macrocytic anemia when:9
- In nonpregnant females, hemoglobin < 12g/dL or hematocrit < 36%
- In pregnant females, hemoglobin < 11g/dL
- In males, hemoglobin < 13 g/dL or hematocrit < 41%.
A history of alcohol abuse is an important indication to the cause of the increased mean cell volume (MCV) and red cell distribution (RDW). Target cells are often observed in macrocytic anemia.9 Although the macrocytosis of alcoholism may be secondary to poor nutrition with a resulting folate or vitamin B-12 deficiency, it is more often due to direct toxic effect of the alcohol on the marrow.8,9 Those who drink excessive amounts of alcohol can develop macrocytosis even in the absence of other factors associated with RBC enlargement, such as alcoholic liver disease or folic acid deficiency. Alcohol abuse is the disorder most commonly associated with macrocytosis: Up to 80% of men and 46% of women with macrocytosis have been found to be alcoholics. The exact mechanism is unknown, however, alcoholism appears to interfere directly with RBC development, because macrocytosis is reversed in the abstinence of alcohol.8
Laboratory Methods for Detection and Identification
Presumptive identification is made by traditional physiological and biochemical methods. On microscopic examination, S. pneumonia bacteria appear as gram-positive cocci arranged in chains and pairs (diplococci). A green, α-hemolytic, zone surrounds S. pneumonia colonies on blood-agar plates. Pneumococci produce pneumolysin, which breaks down hemoglobin into a green pigment that can be observed as a large green zone surrounding S. pneumoniae colonies growing on blood agar plates (Table 2). S. pneumoniae colonies vary in appearance depending on the degree of encapsulation of the organism.10
The opacity variance of S. pneumoniae colonies appears to reflect differences in the organism's pathogenesis and virulence. For example, transparent variants are associated with increased amounts of cell-wall-associated teichoic acid, while opaque variants are associated with enhanced production of capsular polysaccharides.11 Optochin susceptibility test is used to differentiate Streptococci pneumonia from Streptococci viridian's because of its ability to selectively inhibit the growth of S. pneumoniae on blood agar plates at very low concentrations. A zone of inhibition greater than 14 mm with a 6-mm disk or a zone of inhibition or greater than 16 mm with a 10-mm disk is considered susceptible and a presumptive identification of S. pneumoniae. Isolates producing smaller zones should be tested for bile solubility to confirm their identity.10
The test for bile solubility takes advantage of the S. pneumoniae autocatalytic enzyme amidase. The addition of the bile salts or detergent accelerates the natural lytic reaction observed in pneumococcal cultures by increasing the activation of autolytic enzymes produced by Streptococcus pneumoniae. S. pneumoniae in a bile salt solution lyses, and the solution becomes clear. Other α-hemolytic organisms do not undergo autolysis, and the solution remains cloudy.10,11 Additional testing, by serology, may occasionally be necessary, since not all pneumococcal strains lyse completely with the addition of bile salts.11
The Quellung reaction (swelling of the capsule) is considered the “gold standard” technique for serotyping Streptococcus pneumonia and is another means of identification. This microscopic “precipitin test” can be used to identify pneumococci or to determine the capsular serotype of individual pneumococcal isolates. There are over 90 different capsular serotypes of S. pneumoniae. This technique utilizes a high-quality microscope and specific pneumococcal antisera. This method involves testing a pneumococcal cell suspension with pooled and specific antisera directed against the capsular polysaccharide. The antigen-antibody reactions are observed microscopically. A positive Quellung reaction is the result of the binding of the capsular polysaccharide of pneumococci with type specific antibody contained in the typing antiserum.12
Treatment and Vaccination
Pneumococcal infections are usually managed with penicillin however, a growing number of penicillin-resistant S. Pneumoniae strains have caused concern. The organism has developed antibiotic resistance due to its ability to genetically recombine and reproduce rapidly. Other antibiotics that have been show to work well on penicillin-resistant bacteria include erythromycin and chloramphenicol. Physicians have started to use a ‘broad spectrum of antibiotics to treat first and then an antibiotic sensitivity test is performed to identify the best antibiotic. The susceptibility and resistance of S. pneumonia to various antibiotic depends on the geographic region, country, and time.10
Two vaccines are available for prevention of S. pneumoniae and are recommended for infant, elderly or immunocompromised people. The vaccines currently offer protection against the most common strains, but due to the large antigenic variety of the S. pneumoniae, which has more than 90 capsular serotypes identified based on capsular polysaccharides, a universal vaccine has not been developed.10
The pneumococcal conjugate vaccine (PCV13 or Prevnar 13®) protects against 13 types of pneumococcal bacteria. The recommendation by the Center for Disease Control is “PCV13 for use in infants and young children and adults 65 years or older. Older children and adults younger than 65 years old who are at increased risk for getting pneumococcal disease may also need a dose of PCV13.”11,15 The pneumococcal polysaccharide vaccine (PPSV23 or Pneumovax®) protects against 23 types of pneumococcal bacteria. The Center for Disease control recommends it “for all the patient adults 65 years or older and for those 2 years or older at increased risk for disease.”10,13
Even with treatment, some people with pneumonia, especially those in high-risk groups, may experience complications, including bacteremia or sepsis, difficulty breathing, pleural effusion, or lung abscess. Bacteria that enters the bloodstream from the lungs can spread the infection to other organs, potentially causing organ failure. If the pneumonia is severe or if there is chronic underlying lung diseases, the patient may have trouble breathing in enough oxygen. This could lead to hospitalization and use of a breathing machine while the lung heals. Pneumonia may cause fluid to build up in the thin space between layers of tissue that line the lungs and chest cavity. If the fluid becomes infected, it may be necessary to drain it through a chest tube or remove it surgically. An abscess occurs if pus forms in a cavity in the lung. An abscess is usually treated with antibiotics.1,3,13
Summary
Streptococcus pneumoniae is one of the most common organisms causing upper respiratory, lower respiratory, and invasive infections in children and adults. The patient in this case exhibited fever, chills, and deep productive cough, all typical symptoms associated with S. pneumonia. In this case, the increase in white bloods cells, decrease in lymphocytes and increase in neutrophils in addition to the presence of toxic granulation, Döhle bodies, and vacuoles serve as indicators for bacterial-induced infection, such as Streptococcus pneumonia. Additionally, bacterial testing that includes colony morphology, Gram stain, catalase reaction, alpha-hemolytic activity on 5% sheep blood agar, optochin susceptibility, and bile solubility (Table 2) all assist in identification of S. pneumonia as the causative organism for the patient’s fever, chills, and deep productive cough.3,10, More than 90 serotypes have been identified, based on capsular polysaccharides. The Quellung test is another means of identification. Employing all the tests described above can provide a clear identification of S. pneumoniae. Treatment for S. pneumonia is usually penicillin or a “broad spectrum” of antibiotics.
In addition to the S. pneumonia infection the patient also has a macrocytic anemia, based on a history of alcoholism and CBC results (Table 1). In cases of macrocytosis related to alcoholism, the elevated MCV may be due to the direct effect of the alcohol, liver disease, and/or folate deficiency.8,9 Macrocytosis due to alcoholism usually reverses only after a few months of abstinence from alcohol.8
Questions
1. How does pneumonia present in patients with S. pneumoniae infection?
- a. Chills, diarrhea, fatigue
- b. Fever, chills, deep cough
- c. Fever, diarrhea, loss of appetite
- d. Abdominal pains, vomiting, fatigue
- 2. A high white blood count with increased in neutrophils indicates what type of infection
- a. Viral infection
- b. Bacterial infection
- c. Fungal infection
- d. Protozoan infection
- 3. What leukocyte cytoplasmic inclusion is composed of ribosomal RNA?
- a. Primary granules
- b. Toxic granules
- c. Döhle bodies
- d. Howell-Jolly bodies
- 4. What is the “gold standard” test for Streptococcus pneumonia?
- a. Optochin sensitive test
- b. Bile Solubility test
- c. Quellung test
- d. Catalase Test
- 5. Which of the following is the drug of choice for treating most streptococcal infections?
- a. Erythromycin
- b. Cephalothin
- c. Penicillin
- d. Gentamicin
Figures
- [image: https://www.medialabinc.net/courses/imgs/970-326139.jpg] [image: https://p5759554.vo.llnwd.net/e1/courses/imgs/600-663991.jpg] [image: https://www.medialabinc.net/courses/imgs/970-326140.jpg]Image 2 – Döhle Bodies 7
- Image 3 –Vacuoles 7
- Image 1 – Toxic Granulation 7
- References
- Keohane Elaine M, Smith Larry J, and Walenga Jeanine M. Rodak’s Hematology: Clinical Principles and Applications. 5th ed. St. Louis: Elsevier; 2016.
- Grayson Kristina M, Blevins Lance K, Oliver Melisa B, Ornelles David A, Swords W Edwards, Alexander-Miller Marth A. 'Activation-dependent modulation of Streptococcus pneumonia- mediated death in human lymphocytes.' Pathogens and Disease, 2015;75:1-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5827582/pdf/ftx008.pdf.
- Ortqvist Ake, Hedlund Jonas, Kalin Mats. Streptococcus pneumoniae: Epidemiology, Risk Factors, and Clinical Features. Semin Respir Crit Care Med. 2005;26(6):563-574.
- [bookmark: _Hlk3562561]Skovsted Ian C. Textbook in Diagnosis, Serotyping, Virulence Factors and Enzyme-linked Immunoassay (ELISA) for Measuring Pneumococcal Antibodies: Streptococcus Pneumonia, 4th ed. Denmark: SSI Diagnostics; 2017.
- Mitchell AM, Mitchell TJ. Streptococcus pneumonia: virulence factors and variation. Clin Microbiol Infect. 2010;16: 411–418
- Velasco Alonsod Streptococcus pneumoniae: Virulence Factors, Pathogenesis, and Vaccines. American Society for Microbiology. 1995 Dec; 59(4): 591-603. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC239389/pdf/590591.pdf
- Reiqua C. William, Koneman Elmer W. Lab CE MediaLab - White Cell and Platelet Disorders: Peripheral Blood Clues to Nonneoplastic Conditions; c2018 [cited: 2019 March 14]. Available from: https://www.labce.com/white-cell-morphology.aspx
- Ballard Harold S. The Hematological Complication of Alcoholism. Alcohol Health & Research World. 1997; 21(1): 42-52.
- Herrin Vincent E. Emedicine - Medscape Macrocytosis; c2018 [cited: 2019 March 13]. Available from: htps://emedicine.medscape.com/article/203858-overview
- Mahon Connie R, Lehman Donald C. Textbook of Diagnostics Microbiology. 6th ed. St. Louis: Elsevier; 2019.
- Bakdash Suzanne, Couce Marta, Nichols Larry, Pasculle William. Case 349- A man in His 40s with Severe Headaches after a fall; c2003 [cited 2019 March 14] Available from: https://path.upmc.edu/cases/case349.html
- Habib Maha, Porter Barbara D, Satzke Catherine. Capsular Serotyping of Streptococcus pneumonia Using the Quellung Reaction. J Vis Exp Feb 2014; 84; 1-4.
- National Center for Immunization and Respiratory Diseases, Division of Bacterial Diseases. Pneumococcal Vaccination Center for Disease Control. US Department of Health and Human Services. c2017 [cited: 2019 March 14]. Available from: https://www.cdc.gov/pneumococcal/vaccination.html
Question Answers
- - b. Fever, chills, deep cough
- – b. Bacterial infection
- – c. Döhle bodies
- a. Howell-Jolly bodies
- c. Quellung test
- – c. Penicillin





 Stuck on your essay?
Stuck on your essay?

