Introduction of Huntington’s disease
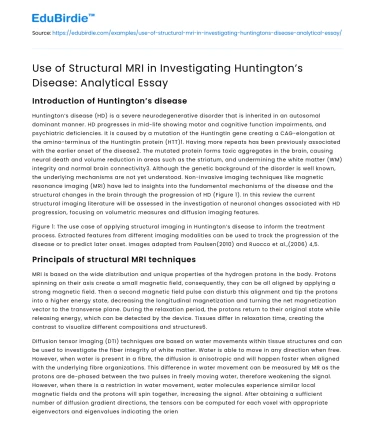
Huntington’s disease (HD) is a severe neurodegenerative disorder that is inherited in an autosomal dominant manner. HD progresses in mid-life showing motor and cognitive function impairments, and psychiatric deficiencies. It is caused by a mutation of the Huntingtin gene creating a CAG-elongation at the amino-terminus of the Huntingtin protein (HTT)1. Having more repeats has been previously associated with the earlier onset of the disease2. The mutated protein forms toxic aggregates in the brain, causing neural death and volume reduction in areas such as the striatum, and undermining the white matter (WM) integrity and normal brain connectivity3. Although the genetic background of the disorder is well known, the underlying mechanisms are not yet understood. Non-invasive imaging techniques like magnetic resonance imaging (MRI) have led to insights into the fundamental mechanisms of the disease and the structural changes in the brain through the progression of HD (Figure 1). In this review the current structural imaging literature will be assessed in the investigation of neuronal changes associated with HD progression, focusing on volumetric measures and diffusion imaging features.
Figure 1: The use case of applying structural imaging in Huntington’s disease to inform the treatment process. Extracted features from different imaging modalities can be used to track the progression of the disease or to predict later onset. Images adapted from Paulsen(2010) and Ruocco et al.,(2006) 4,5.
Save your time!
We can take care of your essay
- Proper editing and formatting
- Free revision, title page, and bibliography
- Flexible prices and money-back guarantee
Principals of structural MRI techniques
MRI is based on the wide distribution and unique properties of the hydrogen protons in the body. Protons spinning on their axis create a small magnetic field, consequently, they can be all aligned by applying a strong magnetic field. Then a second magnetic field pulse can disturb this alignment and tip the protons into a higher energy state, decreasing the longitudinal magnetization and turning the net magnetization vector to the transverse plane. During the relaxation period, the protons return to their original state while releasing energy, which can be detected by the device. Tissues differ in relaxation time, creating the contrast to visualize different compositions and structures6.
Diffusion tensor imaging (DTI) techniques are based on water movements within tissue structures and can be used to investigate the fiber integrity of white matter. Water is able to move in any direction when free. However, when water is present in a fibre, the diffusion is anisotropic and will happen faster when aligned with the underlying fibre organizations. This difference in water movement can be measured by MR as the protons are de-phased between the two pulses in freely moving water, therefore weakening the signal. However, when there is a restriction in water movement, water molecules experience similar local magnetic fields and the protons will spin together, increasing the signal. After obtaining a sufficient number of diffusion gradient directions, the tensors can be computed for each voxel with appropriate eigenvectors and eigenvalues indicating the orientation of elements such as axons. Estimated tensors can be further used to calculate the fractional anisotropy (FA) index that represents how diffusion is directionally constrained in a voxel. Additional outcome measures that directly quantify diffusivities such as mean, radial and axial diffusivity (MD,RD,AD) are often used to describe differences in structural integrity7.
Structural MRI in HD
The most robust pathological change in HD patients are selective neural loss in areas such as the striatum8. The progressive loss can start 15 years earlier than the onset of the disease9. The number of the CAG repeats have been associated with the severity of striatal loss10. Large-scale longitudinal studies such as PREDICT-HD11 and TRACK-HD12 identified the striatal volume and the rate of atrophy as predictors for transfer into late stage HD. Some cross-sectional studies do not agree with TRACK-HD in whether the putamen or caudate changes are more prominent in terms of longitudinal alteration13. These contradictions could originate from different methods being used for outlining the two components of the striatum. As the striatum is important in executing cognitive functions that are usually impaired in HD, the robust volume loss in this area can be used as an effective biomarker13. Significant changes in this area are correlated with other cognitive14 and motor impairment measures14,15. There are some controversies in the literature on whether the rate of change in striatal volumes is consistent throughout the progression of the disease. TRACK-HD reported progressively increasing atrophy rates while other studies present a constant rate after the commencement of atrophy13. This difference could originate from not controlling for age, and differences in methods assessing the rate of change. Some other subcortical structures such as the thalamus, pallidum, and nucleus accumbens were undergoing atrophy during disease progression, however, with smaller effects sizes and less sensitivity16. Automated segmentation techniques might offer an alternative for a more precise outlining of these structures, as defining the outline of these can be challenging. Cortical thinning happens early during the disease and seems to be progressing from posterior to anterior regions of the brain and it is correlated with other clinical measures17. However, the effect sizes are still small compared to the striatum18. An additional important structural change is the degradation in WM around areas affected by the disease. Longitudinal change around striatum19, frontal lobe13 and corpus callosum20 can be followed through disease progression and these changes are associated with deteriorating cognitive measures21. Furthermore, these alterations are strong in predicting future progression of the disorder13. Structural MRI can provide a reliable monitor for longitudinal changes even within short periods of time and can be considered as an outcome measure for clinical trials in disease-modifying treatment studies in the future. The most significant differences have been reported from WM13 and striatum12 which can provide strong effect sizes.
Use of DTI in HD
The previously described findings rely on volumetric changes of brain structures, however, these do not consider microstructural differences. Grey and white matter integrity changes have been mostly quantified by DTI-based metrics to provide a complement to volumetric changes. DTI outcome measures can be used to monitor additional differences between patients and healthy individuals. Moreover, changes in these measures are expected to happen earlier than volume loss, therefore are important in predicting disease advancement. FA can suggest loss of directionality of water flow, possibly due to structural changes, like axonal loss. RD can give a measure of myelin breakdown while AD can represent the changes due to Wallerian degradation. An overall reduction in FA and increase in MD is therefore expected during disease progression. In the striatum of HD patients, an unexpectedly increased FA was reported, that could originate from selective loss of some neuronal connections, making this subcortical structure permanently more organised22. There was a significant increase of MD in the thalamus and putamen that was probably related to prior striatal injuries, as they are part of the same cortico-striatal circuit23. Areas outside this circuit such as corpus callosum that is many form from pyramidal projection also show independent atrophy24. Earlier studies found that in pre-stage patients there was an increase in AD and RD while there is a decrease in FA in corpus callosum25. This supports the idea that both demyelination and secondary effects of grey matter (GM) loss could lead to WM disruptions. In later studies, it was confirmed that changes in AD are mainly present in later stages of the disease26. There have been some controversies on whether WM atrophy is a prominent feature in early stages or just a secondary effect of GM loss. However, it is becoming more evident that there is considerable WM atrophy in multiple areas in both pre and late-stage HD. Combining DTI with quantitative magnetization transfer technique revealed that myelin might play an important role in this process27, while another type of MRI metric (NODDI)28 showed that axonal reduction may underly this pathology. As the tensor measures of DTI are an average for all microstructures within a region, it does not account for individual components. In addition, the outcome measures of DTI might mean a combination of different underlying causes and not just a single aspect. For example, an increase of RD can be interpreted as the loss of myelin in the system, but not exclusively, as axonal loss or crossing of fibers can also contribute to changes in this measure. DTI measures are related to different clinical measures, however, their future use as potential biomarkers is constrained by producing smaller effect sizes when compared to MRI volumetric analysis18.
Conclusions and future directions
In this review, the role of structural MRI was addressed in the investigation of Huntington’s disease. Volumetric changes through the progression of the disorder were most evident in the striatum and white matter, which can be used as future biomarkers in clinical trials to verify the efficacy of disease-modifying treatments, which have the prospect to be faster and more reliable than cognitive measures. When investigating further microstructural changes, white matter atrophy was confirmed as an early contributor to HD and not just a consequence of grey matter loss. Furthermore, abnormal myelin processes might mediate the effect of WM changes in HD. There have been a lot of longitudinal studies conducted in HD, however, the findings are sometimes not consistent, which could be due to different ways of measurement and data analysis methods used. Defining a standard image processing method is essential to unify these longitudinal findings. Furthermore, using a combination of imaging modalities or other clinical measures can become a powerful tool to justify the treatment potency of future drugs.
References
- MacDonald, M. E., Ambrose, C. M., Duyao, M. P., Myers, R. H., Lin, C., Srinidhi, L., Barnes, G., Taylor, S. A., James, M. & Groot, N. (1993) A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington's disease chromosomes. Cell. 72 (6), 971-983.
- Duyao, M., Ambrose, C., Myers, R., Novelletto, A., Persichetti, F., Frontali, M., ... & Gray, J. (1993). Trinucleotide repeat length instability and age of onset in Huntington's disease. Nature genetics, 4(4), 387-392.
- DiFiglia, M., Sapp, E., Chase, K. O., Davies, S. W., Bates, G. P., Vonsattel, J. P., & Aronin, N. (1997). Aggregation of huntingtin in neuronal intranuclear inclusions and dystrophic neurites in brain. Science, 277(5334), 1990-1993.
- Paulsen, J. S. (2010). Early detection of Huntington’s disease. Future neurology, 5(1), 85-104.
- Ruocco, H. H., Lopes-Cendes, I., Laurito, T. L., Li, L. M., & Cendes, F. (2006). Clinical presentation of juvenile Huntington disease. Arquivos de neuro-psiquiatria, 64(1), 5-9.
- Gregory, S., Scahill, R. I., Rees, G., & Tabrizi, S. (2018). Magnetic Resonance Imaging in Huntington’s Disease. In Huntington’s Disease (pp. 303-328). Humana Press, New York, NY.
- Basser, P. J., Mattiello, J., & LeBihan, D. (1994). MR diffusion tensor spectroscopy and imaging. Biophysical journal, 66(1), 259-267.
- Aylward, E. H., Codori, A. M., Barta, P. E., Pearlson, G. D., Harris, G. J., & Brandt, J. (1996). Basal ganglia volume and proximity to onset in presymptomatic Huntington disease. Archives of neurology, 53(12), 1293-1296.
- Stine, O. C., Pleasant, N., Franz, M. L., Abbott, M. H., Folstein, S. E., & Ross, C. A. (1993). Correlation between the onset age of Huntington's disease and length of the trinucleotide repeat in IT-15. Human molecular genetics, 2(10), 1547-1549.
- Paulsen, J. S., Langbehn, D. R., Stout, J. C., Aylward, E., Ross, C. A., Nance, M., ... & Duff, K. (2008). Detection of Huntington’s disease decades before diagnosis: the Predict-HD study. Journal of Neurology, Neurosurgery & Psychiatry, 79(8), 874-880.
- Tabrizi, S. J., Reilmann, R., Roos, R. A., Durr, A., Leavitt, B., Owen, G., ... & Kennard, C. (2012). Potential endpoints for clinical trials in premanifest and early Huntington's disease in the TRACK-HD study: analysis of 24 month observational data. The Lancet Neurology, 11(1), 42-53.
- Aylward, E. H., Nopoulos, P. C., Ross, C. A., Langbehn, D. R., Pierson, R. K., Mills, J. A., ... & PREDICTHD Investigators. (2011). Longitudinal change in regional brain volumes in prodromal Huntington disease. Journal of Neurology, Neurosurgery & Psychiatry, 82(4), 405-410.
- C.K. Jurgens, L. Van De Wiel, A.C.G.M. Van Es, Y.M. Grimbergen, M.N.W. Witjes-Ané, J. Van Der Grond, H.A.M. Middelkoop, R.A.C. Roos, Basal ganglia volume and clinical correlates in ‘preclinical’ Huntington's disease, Journal of Neurology, 255 (2008), pp. 1785-1791
- J.S. Paulsen, P.C. Nopoulos, E. Aylward, C.A. Ross, H. Johnson, V.A. Magnotta, A. Juhl, R.K. Pierson, J. Mills, D. Langbehn, M. Nance, Striatal and white matter predictors of estimated diagnosis for Huntington disease, Brain Research Bulletin, 82 (2010), pp. 201-207
- van den Bogaard, S. J., Dumas, E. M., Acharya, T. P., Johnson, H., Langbehn, D. R., Scahill, R. I., ... & Roos, R. A. (2011). Early atrophy of pallidum and accumbens nucleus in Huntington’s disease. Journal of neurology, 258(3), 412-420.
- Rosas, H. D., Liu, A. K., Hersch, S., Glessner, M., Ferrante, R. J., Salat, D. H., ... & Fischl, B. (2002). Regional and progressive thinning of the cortical ribbon in Huntington’s disease. Neurology, 58(5), 695701.
- Hobbs, N. Z., Farmer, R. E., Rees, E. M., Cole, J. H., Haider, S., Malone, I. B., ... & Roos, R. A. (2015). Short-interval observational data to inform clinical trial design in Huntington's disease. Journal of Neurology, Neurosurgery & Psychiatry, 86(12), 1291-1298.
- Tabrizi, S. J., Scahill, R. I., Durr, A., Roos, R. A., Leavitt, B. R., Jones, R., ... & Kennard, C. (2011). Biological and clinical changes in premanifest and early stage Huntington's disease in the TRACK-HD study: the 12-month longitudinal analysis. The Lancet Neurology, 10(1), 31-42.
- H.E. Crawford, N.Z. Hobbs, R. Keogh, D.R. Langbehn, C. Frost, H. Johnson, B. Landwehrmeyer, R. Reilmann, D. Craufurd, J.C. Stout, A. Durr, B.R. Leavitt, R.A. Roos, S.J. Tabrizi, R.I. Scahill, Corpus callosal atrophy in premanifest and early Huntington's disease, J. Huntingtons Dis., 2 (4) (2013), pp. 517-526
- Beglinger, L. J., Nopoulos, P. C., Jorge, R. E., Langbehn, D. R., Mikos, A. E., Moser, D. J., ... & Paulsen, J. S. (2005). White matter volume and cognitive dysfunction in early Huntington's disease. Cognitive and Behavioral Neurology, 18(2), 102-107.
- Douaud, G., Behrens, T. E., Poupon, C., Cointepas, Y., Jbabdi, S., Gaura, V., ... & Bachoud-Lévi, A. C. (2009). In vivo evidence for the selective subcortical degeneration in Huntington's disease. Neuroimage, 46(4), 958-966.
- Liu, W., Yang, J., Burgunder, J., Cheng, B., & Shang, H. (2016). Diffusion imaging studies of Huntington's disease: a meta-analysis. Parkinsonism & related disorders, 32, 94-101.
- Rosas, H. D., Lee, S. Y., Bender, A. C., Zaleta, A. K., Vangel, M., Yu, P., ... & Salat, D. H. (2010). Altered white matter microstructure in the corpus callosum in Huntington's disease: implications for cortical “disconnection”. Neuroimage, 49(4), 2995-3004.
- Weaver, K. E., Richards, T. L., Liang, O., Laurino, M. Y., Samii, A., & Aylward, E. H. (2009). Longitudinal diffusion tensor imaging in Huntington's Disease. Experimental neurology, 216(2), 525-529.
- Di Paola, Á., Luders, E., Cherubini, A., Sanchez-Castaneda, C., Thompson, P. M., Toga, A. W., ... & Sabatini, U. (2012). Multimodal MRI analysis of the corpus callosum reveals white matter differences in presymptomatic and early Huntington's disease. Cerebral cortex, 22(12), 2858-2866.
- Bourbon-Teles, J., Bells, S., Jones, D. K., Coulthard, E., Rosser, A., & Metzler-Baddeley, C. (2019). Myelin breakdown in human Huntington’s disease: Multi-modal evidence from diffusion MRI and quantitative magnetization transfer. Neuroscience, 403, 79-92.
- Zhang, J., Gregory, S., Scahill, R. I., Durr, A., Thomas, D. L., Lehericy, S., ... & TrackOn‐HD investigators. (2018). In vivo characterization of white matter pathology in premanifest Huntington's disease. Annals of neurology, 84(4), 497-504.





 Stuck on your essay?
Stuck on your essay?

